A disease of non-infectious origin, first, the hyaline cartilage of the knee joint is damaged, eventually collapsing and stopping its function, further causing the destruction of other parts of the joint and causing it to deform.
This degenerative malnutrition usually occurs in women after the age of 40, but men can also be affected, especially those who are overweight, prone to frequent hypothermia, participate in active sports or because of injury.
Of all joint diseases, knee joint disease is the most common.
There is an opinion that the cause of arthropathy is the deposition of salt in the joints. This view is absolutely false, the deposition of salt is a secondary process that causes pain during the development of the disease and is located at the attachment points of tendons and ligaments. Prevention plays an important role in disease prevention.
Knee Anatomy
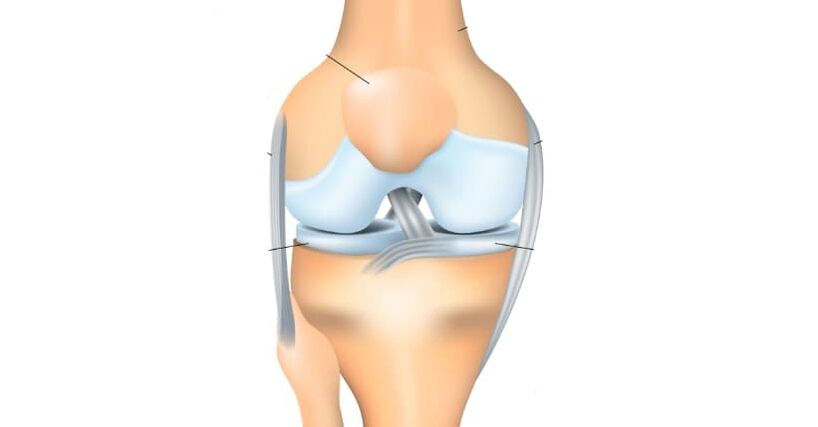
The knee joint consists of two surfaces formed by the tibia and femur. In the front, the knee joint protects the patella, which moves between the femoral condyles. The fibula is not involved in the formation of the knee joint and inherently does not carry any functional load, so it is often used to rebuild other skeletal elements in the body.
All articular surfaces: The inner surfaces of the tibia, femur and patella are lined with hyaline cartilage, which is very smooth and has a high degree of strength and elasticity. This dense and elastic structure is 5-6 mm thick. Cartilage absorbs cushioning during physical activity, preventing friction and reducing impact.
Classification of knee joint disease
In terms of origin, knee arthropathy can be divided into primary, expressive (no injury), and secondary development (caused by trauma, disease, or developmental pathology, often unilaterally). In this case, the first type of arthritis usually occurs in older people and is rarely unilateral.
During its development, arthropathy of the knee goes through the following stages:
- first stage of knee disease- Does not cause significant distress to the patient, characterized by intermittent pain or tightness, especially after strenuous exercise or direct load on the knee joint. There are so-called "pain onset" symptoms, when the patient suddenly stands up, the pain appears, then gradually disappears, but then reappears if a greater load is placed on the limb. There may be slight swelling that goes away on its own. Rarely, but it does occur, synovitis - fluid builds up in the joint pockets of the knee, so the knee area becomes spherical and swollen, limiting movement in the extremities. At this stage, the joints are not yet deformed.
- second stage- The patient begins to suffer from prolonged and rather severe pains on the anterior and medial sides of the joint, which usually disappear after prolonged rest, even if the load is light. As the joint moves, a creaking sound is heard, and if the patient tries to flex the limb as much as possible, severe pain occurs, and the joint movement is limited and deformation begins to be detected. Synovitis occurs frequently, with prolonged disturbances and a large accumulation of fluid in the joints.
- The third phase- Causes considerable distress to the patient, the pain is persistent and interferes not only when walking, but also at rest and even at night, thus preventing sleep. The joints have been significantly deformed, and the position of the limbs has become an X or O shape. When a staggering gait occurs, often due to obvious deformation, people's legs can not be bent or even fully straightened, so they have to rely on crutches or even crutches to walk.
Pathology of Knee Arthropathy

- In the initial stages of arthropathy, the articular surface gradually loses its intrinsic character due to the pathological process of the angiogenesis that supplies the hyaline cartilage within the bone. They start to dry out, lose their smooth texture, cracks appear, so the sliding of the joint surfaces is disturbed, and they start to stick to each other, adding to the surface imperfections. The hyaline cartilage degenerates, losing its shock absorbing function due to continued microtrauma.
- In the second stage of arthropathy, the manifestations of degenerative dystrophy increase: the joint space narrows, the articular surface flattens, adapting to the increased load. The portion of the bone adjacent to the hyaline cartilage of the joint becomes denser, and osteophytes develop along its edges in the form of spike-like growths of bony tissue. The knee capsule also changes and loses its elasticity. The fluid in the joint becomes more and more viscous, altering its nutritional and lubricating properties, further impairing joint function. Due to malnutrition, the state of hyaline cartilage was further aggravated, began to disintegrate, and disappeared completely in some places. Due to the increase in friction, the degeneration of the knee joint gradually increases, leading to the third stage of knee arthropathy.
- In the third stage of knee arthropathy, the range of motion of the joint is significantly limited. The surface is visibly deformed, there is little hyaline cartilage, and the bones appear to be pressed against each other.
Causes of knee joint disease
Essentially, it is impossible to identify any one cause of arthropathy. Basically, its occurrence is the result of a combination of various reasons and various internal and external factors.
In 20-30% of cases, trauma to the knee joint or its components (ligaments, tendons, meniscus) and fractures of the femur or tibia cause knee arthropathy. The disease usually appears 3-5 years after injury. But there are also cases of knee joint disease in the early stage (2-3 months).
In some patients, high-intensity physical exertion can trigger arthropathy. Often, active physical activity can trigger disease, especially after 40 years, when people start exercising actively to stay fit and realize the need for a healthy lifestyle. Most importantly, the load on the joints is when running, as well as jumping and squatting.
Being overweight can also lead to arthropathy, especially in combination with varicose veins in the lower extremities. Increased load on the knee joint, minimally invasive or even severe damage to the meniscus or joint ligaments. In this case, healing is much more difficult because. To lighten the load on the joints, it is impossible to lose excess weight quickly.
Various types of arthritis (gout, psoriasis, rheumatoid, reactive, or Bechterew disease), some neurological disorders (spinal injuries, head injuries, and other disorders that compromise the innervation of the lower extremities), and genetic disorders, canCauses the development of arthropathy, leading to weakness of the connective tissue.
Diagnosis of knee joint disease
For patients diagnosed with knee arthropathy, collection of complaints, examinations and X-rays are necessary.
Today, X-ray images of the joints are the simplest and most accessible research method with which to diagnose patients with sufficient accuracy, observe the development of dynamic processes and determine strategies for further treatment. Among other things, X-rays allow you to make differential diagnoses, such as excluding tumor processes or inflammation in the bone tissue of the thigh or calf. Furthermore, for the diagnosis of knee arthropathy, computed tomography and magnetic resonance imaging are used, which can show changes not only in bone structure but also in soft tissue.
In old age, everyone has certain symptoms of knee joint disease, so the diagnosis can only be made after a complete collection of medical history, chief complaints and visual inspection, and instrumental research methods.
Treatment of knee joint disease
When the first signs of knee disease appear, it is necessary to consult an orthopaedic doctor as soon as possible. During the initial stages of the process, doctors prescribe medication and complete rest of the affected limb.
After the acute phase has subsided, it is possible to specify:
- exercise therapy courses,
- massage,
- as well as physiotherapy procedures (analgesic electrophoresis, UHF therapy, magnetic or laser therapy, anti-inflammatory steroid ultrasound therapy, mud therapy, etc. )
In the next stage of treatment, the doctor may prescribe medication, which includes taking chondroprotective agents that stimulate metabolic processes in the joint. Intra-articular injections with hormone-containing drugs are sometimes required. If the patient has the opportunity to receive convalescent and hydrotherapy treatment, it is recommended to him. Often, to unload the joint, patients are advised to use crutches while walking. You can prevent it with special orthopedic insoles or orthoses.
If a patient is diagnosed with the third stage of knee arthropathy, the most pronounced (pain, impaired joint function, or complete loss of function), surgical treatment, including knee replacement, may be required. Rehabilitation measures until joint function is fully restored, usually 3 to 6 months, after which the patient can return to normal life.
prevention
To avoid degenerative and damaging changes in the knee joint with age, physical education, wearing orthopedic shoes, weight control, and monitoring of rest and exercise regimens are necessary.



















